A perfect storm of private sector profiteering, reckless production practices, environmental destruction and underinvestment in medical research has made global pandemics more common, and undermined our capacity to deal with them.
For a list of sources see the original article from Marxist.com.
While COVID-19 has taken governments worldover by surprise, it was an accident waiting to happen. Just as the economic and social chaos the pandemic has provoked was prepared in the last period, capitalism has long since laid the basis for a public health disaster on this scale.
“You want a vaccine? Show me the money”
 Apologists for capitalism preach the superiority of the free market system over economic planning. But pharmaceutical production and R&D are totally hobbled by market forces. In the past two decades, there have been a number of international viral outbreaks that have claimed thousands of lives (Sars-CoV-1, Mers, Zika, Ebola etc.) To date, only one vaccine for these diseases has reached the market – for Ebola.
Apologists for capitalism preach the superiority of the free market system over economic planning. But pharmaceutical production and R&D are totally hobbled by market forces. In the past two decades, there have been a number of international viral outbreaks that have claimed thousands of lives (Sars-CoV-1, Mers, Zika, Ebola etc.) To date, only one vaccine for these diseases has reached the market – for Ebola.
Coronavirus is not an unknown threat. SARS is part of the coronavirus family. The US government has spent more than £500m on coronavirus research over the past 20 years. However, scientists are starting well behind the curve. Jason Schwartz, professor at the Yale School of Public Health, told the Atlantic earlier this month: “Had we not set the SARS vaccine research programme aside [in 2004], we would have had a lot more of this foundational work that we could apply to this new, closely related virus.” The high-cost, high-reward business model of for-profit medical R&D doesn’t apply well to active pandemics, because the market immediately dries up when the crisis peters out, which means that funding is pulled and research is shelved.
However, it was recently announced that the US National Institute of Allergy and Infectious Diseases (NIAID) received the first candidate for a vaccine against COVID-19. The vaccine has been produced by NIAID in partnership with a company called Moderna, based on research from various universities in the States, Britain and Australia. The approval process is being fast tracked, meaning trials could begin as early as next month. But it will be at least a year before such a vaccine could be mass produced, by which time the pandemic might have burned out – potentially taking millions of lives with it. And even then, NIAID will require another large pharmaceutical company to take on the task of manufacturing the vaccine. This is because the biggest such companies, like Pfizer, Novartis etc. have a stranglehold on the bulk of raw materials, and have consolidated patents on the manufacturing process for vaccines. So far, there is little interest from these pharmaceutical fat cats. This is despite the fact that US Health and Human Services Secretary Alex Azar has stated that any private manufacturer would be allowed to set “reasonable” prices for their product. “We need the private sector to invest,” he said, “price controls won’t get us there.” For millions of people, this vaccine could be a lifesaver – but the capitalists will not invest if there are no profits to be made. The market economy is leaving humanity to its fate.
The majority of pharmaceutical R&D funding comes from the private sector, which accounted for 67 percent of a total $194.2bn invested in the US health sector in 2018, compared to 22 percent by federal bodies and 8 percent by academic and research institutes. Pharmaceutical companies use these high R&D costs as justification for boosting prices of older and generic drugs, to the point that essential medicines like insulin can cost $25 to $100 a vial in the States. In 2015, the president of Turing Pharmaceuticals, Martin Shkreli, caused a scandal by increasing the cost of Daraprim (a drug used in the treatment of AIDS-related conditions) from $13.50 to $750 per pill. Despite the excuse that such windfalls are reinvested in drug development, the vast majority of new medicines are produced by state-funded or subsidised research: including the new candidate vaccine for COVID-19. Rather than advancing medical research and innovation, private pharmaceutical companies mostly use their financial clout to amass patents on medicines developed with public money, flog derivatives of existing drugs at inflated prices and churn out lifestyle drugs like viagra. By using these practices (and benefitting from a liberalisation of anti-monopoly laws in the 1990s), pharmaceuticals became the fastest-growing and highest-profit legitimate industry on earth by the turn of the millenium, raking in $1.2tn USD in 2018 alone.
With so much easy money flowing in, private pharmaceutical companies have little interest in developing new vaccines on their own initiative – especially for active epidemics. The mechanism by which viruses live and propagate is poorly understood by science. Diseases like coronavirus also mutate very quickly into new strains. Vaccine development is a difficult, expensive and time-consuming process, in which returns are never guaranteed. Trevor Jones, director of the Association of the British Pharmaceutical Industry, claimed that it costs $500 million to research and develop a new drug, and drug companies expect to earn back that investment within the first three to five years of sales. The last “blockbuster vaccine” produced in the private sector was Merck’s Gardasil, for use against HPV, which came out in 2006 after a 20-year development cycle. Forbes recently reported on the industry’s “innovation crisis”, outlining the main contradiction at the heart of this sector: profits are going up, but the number of new drugs and vaccines is going down:
“Failing productivity seems like a strange problem in an industry that generates more cash than it can deploy, enjoys unlimited demand and wields monopolistic pricing power. But pharma is not a ‘normal’ business. Each new drug, each clinical trial is an experiment. Development is inherently unpredictable, as reflected in a success rate of 2%… [A] review of data on changes in the value of drugs and industry revenues between 1995 and 2014 did not show the predicted decline. The productivity problem stems not from constraints on opportunity [but] rising costs.”
In short, developing new medicines presents too high of a risk and not enough of an assured profit, meaning drugs companies are devoting their resources to more lucrative avenues, and doing very well. At the same time, private pharma uses its oligarchic power to hamper the development and manufacture of new drugs by anyone else, including the state. The result is that, while the capitalists are still raking it in, the market has left us ill-equipped to deal with crises like the COVID-19 outbreak.
Contradictions and crisis
 With the private sector dragging its feet, many attempts have been made to build up state-run medical R&D. But while state research has received more funding in the advanced capitalist countries in recent years, it still only commands about 5 percent of total spending in the USA, for example. By contrast, military spending takes up 54 percent. And the immense power of the pharmaceutical oligarchy means it can bend government bodies to its will if they conflict with the bottom line. The state doesn’t dictate to capital, but vice versa.
With the private sector dragging its feet, many attempts have been made to build up state-run medical R&D. But while state research has received more funding in the advanced capitalist countries in recent years, it still only commands about 5 percent of total spending in the USA, for example. By contrast, military spending takes up 54 percent. And the immense power of the pharmaceutical oligarchy means it can bend government bodies to its will if they conflict with the bottom line. The state doesn’t dictate to capital, but vice versa.
The last time the US government approved a national vaccination programme was for swine flu in 1976. Four drug firms – Merck’s Sharp & Dohme, Merrell, Wyeth and Parke-Davis – refused to sell to the government the 100 million doses of the vaccine they had manufactured until they got full liability indemnity and a guaranteed profit. And shortly before the COVID-19 outbreak, the Coalition for Epidemic Preparedness Innovations (CEPI) raised $750bn to expedite the development of vaccines to treat new epidemics, with support from countries like Japan, Germany, Canada etc. But private drugs companies on CEPI’s scientific advisory panel (including Johnson & Johnson, Pfizer and Takeda) forced the organisation to back down on the principle that “all countries would have equal and affordable access to CEPI-funded vaccines”. This ensured the capitalists would still be able to turn a healthy profit on any vaccines developed through this fund, in any foreign market.
Two of the biggest impediments to progress in the field of medical research are also the two biggest fetters on the development of capitalist society in general: the nation state and private property. The rise of protectionist tendencies worldwide also affects the drugs market, with nations jealously concealing the results of their latest pharmaceutical research – both state-funded and private. During this COVID-19 crisis, these tendencies have been accelerated. World leaders are hunkering down behind their borders, refusing to share essential resources to fight the pandemic. The Serbian president recently decried the “fairytale” of European solidarity, given the EU laws that prevent the movement of doctors and key medical supplies to non-Schengen countries. He then announced Serbia’s own borders closed to “foreigners”. In truth, solidarity between the Schengen countries has also broken down, with Germany at first banning the export of desperately needed facemasks to countries like Italy. 21 of the 26 Schengen nations have now closed their borders, posing an existential threat to the EU. This madness is the product of a senile system, which has descended into in-fighting precisely when unity is most needed. Viruses know no borders, and the lack of international coordination severely hampers our ability to respond to pandemics.
Recently, students at the University of Sheffield sequenced whole genomes of the coronavirus from UK patients, and are set to make their research public. This is a remarkable achievement that arose from state-subsidised academia. However, there is now a race to develop a vaccine based on such research, and by various governments to secure exclusivity. First into the dog pile was US President Donald Trump, who followed his ‘America First’ maxim by offering the German biopharmaceutical company CureVac “large sums of money” for exclusive rights to a COVID-19 vaccine and antiviral agents. The German government has apparently met this move with a counter-offer. This could potentially set off a bidding war, which will force millions of people and state health services to buy vaccines at prices set by the winner.
Under a planned world economy, all of the planet’s resources could be pooled into developing an effective treatment and vaccine for COVID-19. But the antagonised interests of capitalist nations prevent this. Attempts to overcome these antagonisms on a capitalist basis have met with little success. For instance, the WHO operates the Pandemic Influenza Preparedness (PIP) Framework, which facilitates the sharing of medical research between nations. But it only applies to influenza, not any other infectious disease with pandemic potential, due to pressure from the industry and governments. Indeed, the WHO itself is a shadow of its lofty objectives. Its funding has been cut in half by the Trump administration, it is rife with rumours of corruption, and has been supplanted by the World Bank as the biggest financier of public health globally. Similar bodies like the Centres of Disease Control and Prevention (CDC) have also seen their budgets slashed in recent years: casualties of the protectionist tendency in the world markets.
Furthermore, private-sector medical companies consider their products (whether they actually developed them, or merely purchased the patents) to be their private possessions: valuable only for their market potential, not their capacity to cure people. Recently, a private company threatened with legal action two volunteers who were 3D-printing valves for use in ventilators, selling them for $1 against a typical market price of $11,000. This kind of private sector parsimony is replicated across the international pharmaceutical market. For example, the 1994 Agreement on Trade-Related Aspects of Intellectual Property Rights (TRIPS) guarantees IP protection for all companies, including pharmaceutical firms, when selling their products in any WTO country. This proves problematic in poorer countries, where essential drugs are the intellectual property of private companies, whose exorbitant prices are too high for these markets, and who resist attempts to produce cheaper derivatives domestically. In response to this problem, in 2001 (on the initiative of the WHO), the Doha Declaration on TRIPS and Public Health – agreed by all WTO Member States – affirmed that public health should always take precedence over the enforcement of intellectual property rights. However, according to Oxfam in 2019: “rich countries and pharmaceutical companies have ignored the Doha Declaration and pursued an aggressive agenda to subject the developing world to even stricter IP protection, through free-trade agreements and unilateral pressure.” In short, powerful nations will always crush the weak, and the private property rights of the capitalists always trump human need.
A recent statement by the British government inadvertently exposed the failure of the so-called free market to ameliorate this pandemic. The Tory administration has banned the parallel export of 80 drugs (including Aluvia, adrenaline and morphine), due to speculation by private companies, which were attempting to buy the drugs cheaply in Britain, then hoard and sell them at an inflated price abroad. This hasn’t been prohibited because it is ethically unacceptable, but because the government was afraid it would “aggravate supply problems”. It has also transpired that the US firm Rising Pharmaceuticals increased the price of chloroquine (an antimalarial, which is being tested against COVID-19) on 23 January, when the scale of the outbreak in China became apparent. The drug price rose 97.86 per cent to $7.66 per 250mg pill and $19.88 per 500mg pill. Although the PR backlash led them to quickly return the cost to the ‘normal’ market rate, Rising has previously been fined for price fixing, and it is clear they intended to exploit the suffering of millions of people to score a windfall. This won’t be the last time a company seeks to turn a quick buck on the coronavirus pandemic.
Contrast this with Cuba’s production and distribution of Interferon alfa 2b: developed in 1986 by the state-run BioCubaFarma in collaboration with China. This drug, which can help stop some of the symptoms of coronavirus, has been tested with positive results on 1,500 coronavirus patients in China already. Cuba has shipped Interferon in large quantities to badly-affected countries like Italy. Teams of Cuban doctors have also been sent to dozens of countries to help fight outbreaks. It is a clear testament to the superiority of a planned economy that a small Carribean Island can produce an effective treatment for a disease that resists the best efforts of the mightiest capitalist countries on earth, and freely send medical resources to those in need. Similarly, whereas for-profit pharmaceutical companies have dropped research into complex conditions like Alzheimer’s disease due to a lack of returns, Cuba’s state-run medical research has produced some exciting breakthroughs against both Alzheimer’s and HIV. Needless to say, the trade embargoes imposed on Cuba by the US will be an obstacle to any of these potentially life-saving treatments reaching the people who need them, and there will be consequences for any US trade partners who accept them.
In one of Italy’s darkest hours, they find they are not alone. Cuban doctors arrive in Italy with one mission, to save as many lives as they can. pic.twitter.com/K7r3DWqy8r
— P KELLY (@7815PWK) March 22, 2020
The limitations of the capitalist system mean that medical R&D on vaccines for serious, life-threatening diseases have been basically stagnant since the 1960s. Humanity is increasingly vulnerable to global epidemics (for reasons I will explain), and our weapons to resist them are becoming obsolete. The pharmaceutical industry is privatising the profits of this essential sector, and socialising the risks. And capitalist governments are facilitating them. An infectious disease researcher interviewed in the New York Times recently opined: “What matters more to the drug companies? Keeping trade secrets and boosting the bottom line or taking a leading role in stemming the COVID-19 outbreak?” The answer is clear as day. A crisis like the current pandemic offers no better argument for placing these unproductive parasites under democratic control so their immense resources can be put to good use.
The poorest suffer most
 So far, COVID-19 has only just hit the least-developed countries. The first confirmed cases have recently been reported in Somalia and Tanzania. Another was detected in the Gaza Strip. The virus will inevitably spread, and when it does, the results will be catastrophic. How can a country like Somalia – which barely has a functioning government, and whose housing and sanitation are in a miserable state – carry out social distancing measures or subsidise lost wages? How will its medical infrastructure cope with thousands of infected patients? And aside from these poor countries, what happens when the thousands of Middle-Eastern refugees living in tents in European migrant camps become infected? The answer is obvious. There will be no containment, there will be no concerted medical response. People will be left to fend for themselves. This state of affairs is merely par for the course when it comes to disease prevention in underdeveloped nations.
So far, COVID-19 has only just hit the least-developed countries. The first confirmed cases have recently been reported in Somalia and Tanzania. Another was detected in the Gaza Strip. The virus will inevitably spread, and when it does, the results will be catastrophic. How can a country like Somalia – which barely has a functioning government, and whose housing and sanitation are in a miserable state – carry out social distancing measures or subsidise lost wages? How will its medical infrastructure cope with thousands of infected patients? And aside from these poor countries, what happens when the thousands of Middle-Eastern refugees living in tents in European migrant camps become infected? The answer is obvious. There will be no containment, there will be no concerted medical response. People will be left to fend for themselves. This state of affairs is merely par for the course when it comes to disease prevention in underdeveloped nations.
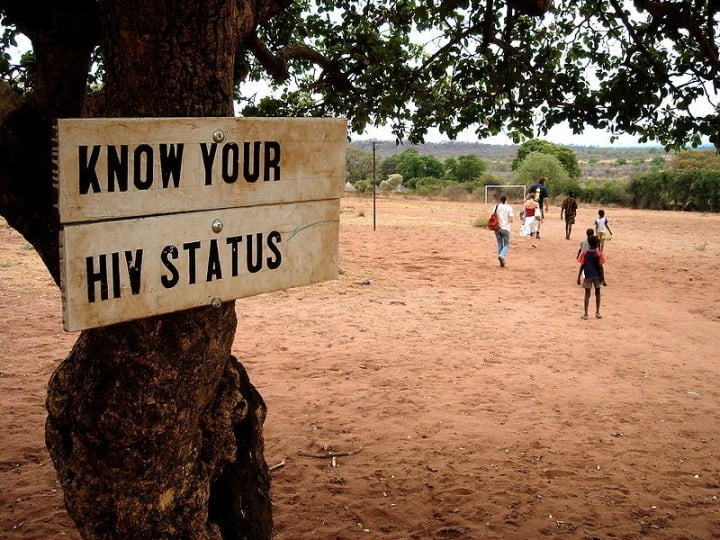
Less than 10 percent of global health research public spending is dedicated to diseases that affect the poorest 90 percent of the world population. Deadly diseases like HIV/AIDS and tuberculosis thrive in poor countries. Neglected tropical diseases kill 500,000 people in the developing world every year. And if private drugs companies see scant financial incentive in developing medicines for the advanced capitalist countries, they see none at all in the poorest nations. Dr. Harvey Bale Jr., head of the International Federation of Pharmaceutical Manufacturers, asserted that there was “no marketplace to speak of in the poor world”. Dr. Bernard Pécoul of the Médecins Sans Frontières added that the push for profits “leaves you focused on 300 to 400 million people in rich countries.” This is a very clear example of where production for profit is grossly misaligned with need.
To give an example, in the late ‘90s, the genome for tuberculosis was sequenced. TB causes terrible suffering in the poorest parts of the world. Despite the WHO organising a 1998 summit to gain the support of leading pharmaceutical companies to develop a vaccine and treatments, none of these companies was willing to commit to any project that would realistically yield profits of less that $350m a year or five years or more. That would have required a total cost of $11 USD per pill, per patient in sub-Saharan Africa, for instance, which at the time spent less than $10 USD per citizen, per year, on all healthcare needs. In short, private pharma refused to commit any of its resources to alleviating the suffering of poor nations unless they accomplished the impossible. The project was abandoned. And aside from a lack of investment in R&D, many private firms have abandoned production of existing, important drugs for the developing world, including five treatments for African sleeping sickness, aminosidine for the parasitic disease leishmaniasis and even the polio vaccine. Far from advancing human society in the fight against illness, capitalism is actually taking us backwards.
International bodies like the WHO and the G8 have attempted to incentivise private sector investment in the poor world with subsidies like Advanced Market Commitments (AMC), through which advanced capitalist countries agree to meet some of the costs of getting affordable vaccines to where they’re needed most. Alternatively, the US Food and Drug Administration offers vouchers that can be exchanged for fast-tracked reviews of any future product to companies that develop effective medicines for neglected diseases. But all of these rewards have failed, either because they don’t provide enough of an incentive, or because pharmaceutical companies have found ways to game the system and enrich themselves even further. For instance, by applying the aforementioned voucher to the anti-malarial medicine Coartem, Novartis accrued an additional profit of $321m solely for registering their product with the US FDA, even though the medicine is already in widespread use elsewhere.
The only value private pharma sees in the developing world is a testing lab to outsource its clinical trials, which represent the single-biggest cost of drug development. This cost can be significantly off-set by exploiting test subjects in places like India, where clinical trials have created a thriving market. Better yet, these firms can often avoid disagreeable red tape like ethical standards and informed consent by moving these operations to countries where regulations are looser, and turning desperate people into their lab rats.
Some poorer countries have sought to offset rising drug costs by investing in their own pharmaceutical manufacture and distribution channels, at the cost of deepening their foriegn debt. However, these efforts have been frustrated by the Pharmaceutical Manufacturers’ Association (the industry’s main bosses’ organisation), which feels this represents an “infringement on their free market rights.” From 2008 to 2018, an Intergovernmental Working Group on Public Health, Innovation and Intellectual Property Rights (IGWG) has sought to address the demands of developing countries for a global system of R&D that better reflects their needs. But its recommendations have been totally ignored by both imperialist countries and private pharma. The situation was summed up in a damning report by Oxfam:
“The lack of medical innovation is a global problem which requires a significant increase in resources, applied in an effective and coordinated manner. The current system of R&D under-utilises the capacities, skills, and resources available in all countries. Efforts to improve R&D across the developing world are fragmented, unsustainable, and unlikely to lead to large-scale changes.”
Despite the complaints of Oxfam and the IGWG, you can’t change the rules of capitalism by appealing to the capitalists’ better nature. If there’s no profitable market, they won’t invest. The reforms they propose would require a fundamental break with the current system. Naturally, research on life-saving treatments for illnesses that afflict the developing world would also have a positive impact on the development of vaccines and treatments in the advanced capitalist countries. But the market system only thinks about immediate returns. Human lives are small change.
Disease also serves to keep the poor world poor. The HIV/AIDS crisis (the origins of which lie in primate-to-human transmission through the illegal bushmeat market, to which desperate populations resorted after successive famines) carved through the developing world like a scythe in the 1980s and 1990s. Up to 121m fewer people are alive today as a consequence of this pandemic. The World Bank estimated in 1991 that HIV/AIDS commanded more than 4 percent of Tanzania’s health budget, 7 percent of Malawi’s, 9 percent of Rwanda’s, 10 percent of Burundi’s and 55 percent of Uganda’s. Furthermore, epidemics in poor nations in Africa and the Americas have been exacerbated by the impact of war and coups, provoked by imperialist meddling, which crippled these countries’ already vulnerable health infrastructures. Insulting attempts from the 1970s by the World Bank to “pressurise” poor countries to spend more on disease prevention and healthcare have been curtailed by their need to service immense debts to bodies like the IMF. Imperialism has brought ruin to these nations, not only through colonialism, exploitation and war, but also illness. Now, they are practically defenceless against emergencies like the COVID-19 pandemic.
Environmental destruction and intensive farming: rearing disease
 While its exact origins are unclear, COVID-19 is thought to have been introduced from animal to human populations at the end of last year in Wuhan, the capital of Hubei province in China, and subsequently spread through national and international travel during Chinese New Year. This is similar to the 2003 SARS outbreaks, which resulted from transmission of a mutated strain of coronavirus at a live animal market in Guangdong province. Neither of these outbreaks were ‘natural’ occurrences. Rather, they were the inevitable consequence of rapacious capitalist production, which is creating fertile ground for potentially lethal diseases to cultivate in animal populations and spread to human beings.
While its exact origins are unclear, COVID-19 is thought to have been introduced from animal to human populations at the end of last year in Wuhan, the capital of Hubei province in China, and subsequently spread through national and international travel during Chinese New Year. This is similar to the 2003 SARS outbreaks, which resulted from transmission of a mutated strain of coronavirus at a live animal market in Guangdong province. Neither of these outbreaks were ‘natural’ occurrences. Rather, they were the inevitable consequence of rapacious capitalist production, which is creating fertile ground for potentially lethal diseases to cultivate in animal populations and spread to human beings.
The increased prevalence of pandemics in recent years can be partly explained by capitalist destruction of the environment. Since 1940, there have been hundreds of microbial pathogens appearing in new territory: including HIV and Ebola in Africa, Zika in the Americas and so on. More than two-thirds of these originate from wildlife, rather than domestic animals. Deforestation through logging, urban expansion, road building and mining destroys wild species’ habitats and increases their contact with human settlements, which offers more opportunities for microbes that live harmlessly in their bodies to “spillover” into ours. Disease ecologist Thomas Gillespie, interviewed in Scientific American stated: “I am not at all surprised about the coronavirus outbreak. The majority of pathogens [in the bodies of wild animals] are still to be discovered. We are at the very tip of the iceberg.”
For example, the 2017 Ebola outbreaks originated from species of bats, who have been forced to roost in trees in farms and backyards due to deforestation. These animals become carriers for animal-to-human strains of viruses due to repeated contact, and either pass on pathogens through bites, fecal matter, or through being sold as food in informal “wet markets” – where species that would never naturally encounter one another are caged side by side. These markets are an essential food source for poor people in Asia and Africa, however, according to Gillespie they are “a perfect storm for cross-species transmission of pathogens. Whenever you have novel interactions with a range of species in one place, whether that is in a natural environment like a forest or a wet market, you can have a spillover event.” This is exactly what resulted in the mutant coronavirus that caused the SARS epidemic, and possibly COVID-19. One hypothesis is that the virus was passed from a bat or pangolin at a wet market to its first human victim: a 55-year-old man.
However, this is only one scenario in which dangerous pathogens can arise from animals. In factory farms, hundreds of thousands of individuals are packed in cramped conditions, which creates an ideal environment for microbes to become lethal pathogens. Bird flu, for example, originated in wild waterfowl. But when the influenza reaches factory farms for chickens, it ravages the population and mutates quickly to become more virulent. This is what produced the feared H5N1 strain of avian influenza, which can infect and kill humans. Moreover, attempts to maximise the production of particular animal products have resulted in the widespread emergence of monoculture farms – in which only one kind of animal is reared. This creates an ideal environment for the evolution of dangerous viruses. Swine flu originated from monocultures of pigs, for example – although the hog farming industry lobbied the WHO to rename swine flu by its scientific name, H1N1, to divert attention from its origin. It has been hypothesised by some scientists that pig monocultures may even have bred the novel coronavirus.
These issues affect agribusiness in all advanced capitalist countries, and food production operations in the US and Europe have served as ground zeroes for the H5N2 and H5Nx influenzas, both of which were downplayed by American public health officials. However, it is no accident that a number of serious epidemics in the past several years have originated from China. Here, as well, capitalist production is to blame.
The rapid development of China’s economy on a capitalist basis has erected an epidemiological house of cards in the country. Rob Wallace’s book, Big Farms Make Big Flu: Dispatches on Influenza, investigates the emergence of avian flu in China. He explains how, in the 1980s and ‘90s, the country modernised and consolidated its agribusiness in provinces like Guangdong, where the first H5N1 case was recorded in 1997. Foreign companies like Charoen Pokphand (CP) were invited to set up shop in Guangdong, introducing vertically integrated operations where the animals, their feed and processing plants were all provided by the same firm. This resulted in an explosion of the number of ducks and chickens produced annually. US-style intensive farming techniques (with even-more-relaxed regulation) were introduced to satisfy market demand and maximise profits, and the insurmountable competition devastated rural agricultural production by peasant communities, leading to a massive internal migration to these provinces. This placed huge monocultures of poultry in close contact with densely packed human populations. Hubei is China’s sixth-largest poultry producing province, with a population of 58.5m. No matter how COVID-19 originated, Hubei was always a ticking time-bomb for disease.
 The immense economic power of companies like CP (which now produces 600m of China’s 2.2bn chickens annually sold) translates into huge political power in Asia, which comes in useful when their actions result in pandemics. For instance, CP was a major supporter of Telecommunications tycoon Thaksin Shinawatra, the prime minister of Thailand during the country’s first bird flu epidemic – whose promises to run the country “like a business” saw massive attacks on workers’ rights and aggressive liberalisation of the Thai economy. When the outbreaks began in Thailand, Shinawatra played an active role in blocking efforts to stem the spread of bird flu. Chicken-processing plants actually intensified production, with trade unionists reporting that one factory was still churning out between 90,000 to 130,000 poultry daily, despite it being obvious the chickens were sick. Shinawatra and his ministers went on TV eating chickens to show their confidence, but behind the scenes, CP and other big agribusinesses were colluding with the government to pay off contract farmers to keep quiet about their infected flocks. In return, the government was secretly supplying corporate farmers with vaccines, while poorer farmers were kept in the dark: putting themselves and their animals at risk. When Japan banned poultry from China during the crisis, CP’s Thai factories picked up the slack, resulting in the company making even-greater profits from an epidemic largely of its own making!
The immense economic power of companies like CP (which now produces 600m of China’s 2.2bn chickens annually sold) translates into huge political power in Asia, which comes in useful when their actions result in pandemics. For instance, CP was a major supporter of Telecommunications tycoon Thaksin Shinawatra, the prime minister of Thailand during the country’s first bird flu epidemic – whose promises to run the country “like a business” saw massive attacks on workers’ rights and aggressive liberalisation of the Thai economy. When the outbreaks began in Thailand, Shinawatra played an active role in blocking efforts to stem the spread of bird flu. Chicken-processing plants actually intensified production, with trade unionists reporting that one factory was still churning out between 90,000 to 130,000 poultry daily, despite it being obvious the chickens were sick. Shinawatra and his ministers went on TV eating chickens to show their confidence, but behind the scenes, CP and other big agribusinesses were colluding with the government to pay off contract farmers to keep quiet about their infected flocks. In return, the government was secretly supplying corporate farmers with vaccines, while poorer farmers were kept in the dark: putting themselves and their animals at risk. When Japan banned poultry from China during the crisis, CP’s Thai factories picked up the slack, resulting in the company making even-greater profits from an epidemic largely of its own making!
Another long-term threat posed by intensive farming (to which I will return later) is the cultivation of antibiotic resistant microbes. Shortly after the discovery of antibiotics revolutionised medical science, it was discovered that expensive livestock lived longer when dosed with them. Unfortunately, livestock undergoing these treatments place more than double the global selective pressure on bacterial populations to evolve and become resistant, which exacerbates an existing, and already extremely serious problem for public health.
In short, the massive pressure placed on animals and the environment by capitalist production has contributed to a very dangerous scenario, in which human-communicable pathogens are evolving and spreading at an accelerated rate. It recalls the words of Engels, writing in Dialectics of Nature:
“Let us not…flatter ourselves overmuch on account of our human victories over nature. For each such victory nature takes its revenge on us. Each victory, it is true, in the first place brings about the results we expected, but in the second and third places, it has quite different, unforeseen effects which only too often cancel the first…”
Nowhere is this sentiment truer than in the pathogens that originate in factory farms. However, none of the problems outlined here are endemic to efficient food production. All of them stem from intensive farming techniques, designed to maximise profits above all, which are very cruel to the animals we eat, and potentially disastrous to public health. There is no reason that monocultures of animals, dosed on antibiotics, must be crammed cheek-by-jowl into hellish factories, and become breeding grounds for disease. Under a rationally planned economy, all of these processes could be made as efficient, humane and safe as possible, without having to satisfy the capitalists’ lust for profits.
“Outbreaks are inevitable, pandemics are optional”
 In 1994, Pulitzer-winning journalist Laurie Garrett wrote The Coming Plague: Newly Emerging Diseases in a World Out of Balance. This was followed in 2001 by Betrayal of Trust: The Collapse of Global Public Health. Over these two books, she explained that “human disruption of the global environment, coupled with behaviors that readily spread microbes between people and from animals to humans, guaranteed a global surge in epidemics, even an enormous pandemic. [These] outbreaks were aided and abetted by inept health systems, human behavior, and the complete lack of consistent political and financial support for disease-fighting preparedness everywhere in the world.” Though she didn’t put it in these terms, these books were a damning indictment of capitalism and its corrosive effects on public health. Garrett’s warnings were corroborated in a 2018 report by the Global Preparedness Monitoring Board, which warned that “there is a very real threat of a rapidly moving, highly lethal pandemic of a respiratory pathogen killing 50 to 80 million people and wiping out nearly 5% of the world’s economy”.
In 1994, Pulitzer-winning journalist Laurie Garrett wrote The Coming Plague: Newly Emerging Diseases in a World Out of Balance. This was followed in 2001 by Betrayal of Trust: The Collapse of Global Public Health. Over these two books, she explained that “human disruption of the global environment, coupled with behaviors that readily spread microbes between people and from animals to humans, guaranteed a global surge in epidemics, even an enormous pandemic. [These] outbreaks were aided and abetted by inept health systems, human behavior, and the complete lack of consistent political and financial support for disease-fighting preparedness everywhere in the world.” Though she didn’t put it in these terms, these books were a damning indictment of capitalism and its corrosive effects on public health. Garrett’s warnings were corroborated in a 2018 report by the Global Preparedness Monitoring Board, which warned that “there is a very real threat of a rapidly moving, highly lethal pandemic of a respiratory pathogen killing 50 to 80 million people and wiping out nearly 5% of the world’s economy”.
The report continues:
“Between 2011 and 2018, WHO tracked 1,483 epidemic events in 172 countries. Epidemic-prone diseases such as influenza, severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), Ebola, Zika, plague, yellow fever and others, are harbingers of a new era of high-impact, potentially fast-spreading outbreaks that are more frequently detected and increasingly difficult to manage… Any country without basic primary health care, public health services, health infrastructure and effective infection control mechanisms faces the greatest losses, including death, displacement and economic devastation.”
n other words, the current COVID-19 crisis is part of a new era in which pandemics will become more common, for the reasons I have described. The world is underprepared for this, and the poorest countries are going to suffer the most. Aside from the emergence of new pathogens, there are other threats on the horizon, including antibiotic-resistant strains of microbes like streptococcus and staphylococcus, cultivated in hospitals in the advanced capitalist countries, due to an over-reliance on antibiotics developed in the post-war period. Illnesses of the 19th and 20th century, like TB, are returning with a vengeance in poor communities like Harlem in New York City – and developing antibiotic resistance. In the 1990s, a forecast by the University of California predicted that by 2070 the world would have exhausted all antimicrobial drug options, as viruses, bacteria, parasites and fungi would have evolved complete resistance to the human pharmaceutical arsenal. This apocalyptic scenario could be avoided, if more was invested in R&D for vaccines and alternative treatments. But as explained, this is not a profitable avenue for big pharma.
In other words, the current COVID-19 crisis is part of a new era in which pandemics will become more common, for the reasons I have described. The world is underprepared for this, and the poorest countries are going to suffer the most. Aside from the emergence of new pathogens, there are other threats on the horizon, including antibiotic-resistant strains of microbes like streptococcus and staphylococcus, cultivated in hospitals in the advanced capitalist countries, due to an over-reliance on antibiotics developed in the post-war period. Illnesses of the 19th and 20th century, like TB, are returning with a vengeance in poor communities like Harlem in New York City – and developing antibiotic resistance. In the 1990s, a forecast by the University of California predicted that by 2070 the world would have exhausted all antimicrobial drug options, as viruses, bacteria, parasites and fungi would have evolved complete resistance to the human pharmaceutical arsenal. This apocalyptic scenario could be avoided, if more was invested in R&D for vaccines and alternative treatments. But as explained, this is not a profitable avenue for big pharma.
Responding to the aforementioned GPMB report, Garrett was sceptical that any of its proposals (which amount to lobbying governments and private enterprise to cooperate more effectively on funding and research) would amount to anything. She wrote: “With no intention of degrading the GPMB’s effort, I must sadly say that this core message has been shouted from the rafters many times before, with little discernible impact on tone-deaf political leaders, financial enterprises, or multinational institutions. There’s no reason to think this time will be any different.”
Indeed, on a capitalist basis, it is unlikely that the situation will improve. These diseases have been conjured up by the system itself, and the living patterns of modern capitalist societies create ideal conditions for them to spread. Urbanisation has concentrated the vast majority of the planet’s 8bn people into dense populations, where disease can run rampant. And the dramatic increase in worldwide movement of people and goods (facilitated by modern transport, and exacerbated by war and climate change) creates viable channels for microbes to rage across the planet. It only took a matter of days before COVID-19 had spread from one end of the earth to the other. Such a global problem requires an international solution. But, as described, antagonism between different capitalist nations, the private property rights of the major pharmaceutical companies and the profit-based mode of production prevents the kind of coordinated response necessary to fight pandemics.
The capitalist upswing in the postwar period was a period of great optimism for public health. Improved housing and sanitation, and the discovery of antibiotics, meant life expectancies increased sharply. In the United Kingdom, the working class returned from a victorious war demanding reforms, amongst which was the National Health Service: providing complex medical aid freely at the point of use. In 1995, Dr. Jonas Salk’s polio vaccine successfully reduced cases of the illness in Western Europe and North America from 76,000 in 1955 to 1,000 in 1967. In 1978, the WHO convened a meeting of health ministers from over 130 nations in Alma-Ata in the USSR, issuing a document (‘the Declaration of Alma-Ata’) that called for “the attainment by all peoples of the world by the year 2000 of a level of health that will permit them to lead a socially and economically productive life,” defining health as “a state of complete physical, mental, and social well-being, not merely the absence of disease or infirmity,” and “a fundamental human right.” But today, far from a human right, decent and affordable healthcare is denied to millions of people. Meanwhile, years of underinvestment and privatisation have brought progress on medical research to a near-halt, and the democratic gains of the post-war period have been curtailed. The ruling class has met this current crisis with a Malthusian cynicism worthy of Trevelyan, openly considering the “positive economic effects” of COVID-19 killing off “non-productive” layers of society.
The austerity that followed the 2008 crash has taken a heavy toll on public health, the consequences of which are now being ruthlessly exposed by the new coronavirus outbreak. Everywhere, a lack of (privately manufactured) testing kits makes it impossible to gather accurate data on the extent of the coronavirus pandemic. Beds are in critically short supply. Retired health workers are being returned to service. Countries like Britain initially downplayed the risk posed by the virus, before u-turning and imposing a lockdown. The early talk of “mitigation” and “flattening the curve” rather than containment was partly to avoid disrupting business, but was also because the health service can’t take the burden of an outbreak that could reportedly last until 2021 and put 8m people in hospital. Meanwhile, decentralisation and successive cuts to the Italian healthcare system over the last 30 years have led to major shortages of not just ventilators and beds, but even face masks and hand sanitiser, in one of the worst-affected countries. Oversubscribed Italian hospitals have no choice but to choose who lives or dies based on age. Health workers are completely overstrained, with images of Italian nurses passed out from exhaustion testifying to the dire state of affairs. Moreover, the bosses in one country after another are refusing to take appropriate safety measures or cease production until forced to by strike action. And even where bourgeois governments have agreed to underwrite wages and take ownership of certain sectors in order to save the capitalist system, the working class will inevitably be expected to foot the bill when the dust settles. Capitalism has not only made new outbreaks more likely, but has strip-mined public health to the point that it is unable to cope with them.
As the epidemiologist Larry Brilliant, who led the fight against smallpox, once said: “outbreaks are inevitable, but pandemics are optional.” None of this has to happen. Under a planned economy, all the ingenuity of humanity would be directed towards developing vaccines for the biggest killer diseases. Mass immunisation programmes would then be freely conducted in every country on earth – eradicating diseases like Ebola just like we did smallpox. The environmental crises and intensive farming techniques that create breeding grounds for pathogens could be replaced with production planned in harmony with nature, which prioritises human and animal welfare over profits. Any new viral outbreak could be met with a concerted, global response to prevent it from reaching pandemic levels. All research and resources for the treatment of infected cases could be shared and utilised on the basis of need. Rather than having to pay private pharmaceutical companies through the nose, their immense operations would be expropriated and managed on a democratic basis to produce vaccines and antigens as needed. Instead of wasting millions in public money to obtain hospital beds, these could be simply requisitioned. Testing and quarantine facilities could be erected to manage the emergency. And rather than antagonistic capitalist countries racing to hoard resources – and striving to keep business profitable at the expense of public health – federated socialist countries could present a united front against epidemics. Non-essential production could be halted and social distancing measures carried out whenever necessary, without any impact on pay. And logistics could be planned to ensure shelves were stocked, basic necessities were distributed and nobody felt the need to horde essentials.
Modern medicine represents a phenomenal victory of human society over nature. At least in the advanced capitalist countries, it has doubled our life expectancy and massively improved our quality of life. Any modern society that cannot guarantee its population good health, and protection against preventable pandemics, cannot be considered civilised. Where the capitalists and their political cronies meet public health emergencies by shrugging their shoulders and informing the masses: “your loved ones will die”, a socialist society would equip humanity with the weapons it needs in the battle against disease. The callous, inept response of capitalist governments to the COVID-19 pandemic, and the resulting social fallout, will provoke a leap forward in the consciousness of the masses. Already, there have been spontaneous strikes in Italy, Spain, Portugal, France, the USA, Canada and elsewhere against attempts by the bosses to force workers to choose between risking infection at their workplaces, or losing pay. This is only a harbinger of what is to come. We are entering into a new epoch of dramatic struggle against a terminally sick system.